Welcome to Perception from the
Southern California Eye Institute (SCEI).
In this and future issues, we will bring you
promising developments in eye disease
and eye care worldwide.

Dr. Rohit Varma
Founding Director, SCEI
The Bionic Eye:
Restoring Sight
Science, a biology-driven technology company focused on the brain, has designed a visual prosthesis called the Science Eye that may restore vision, in a limited form, in people with retinitis pigmentosa.
CEO Max Hodak co-founded the startup after working at Elon Musk's Neuralink. Other companies, such as GenSight Biologics in Paris and Bionic Sight in New York, also are experimenting with techniques to restore sight.
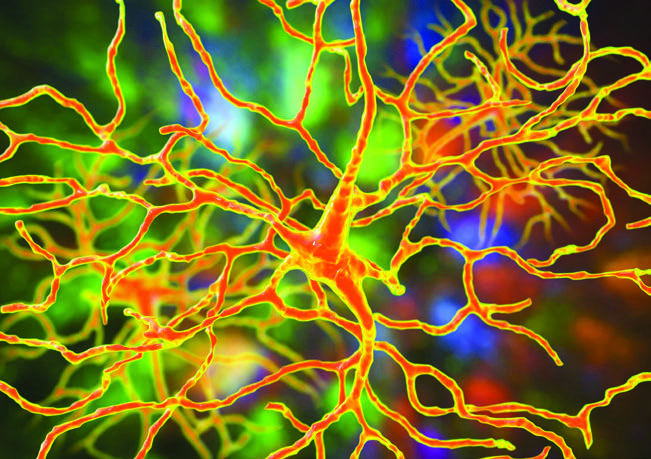
The foundation of their work is optogenetics, which uses a genetically engineered virus to deliver a gene to specific optic nerve cells in the retina, the light-sensitive layer of tissue at the back of the eyeball.
Hodak says clinical trials should begin in the next 18 months. The company is also investigating ways to use gene therapy for macular degeneration.
Improving Research Access for Asians
Alzheimer's disease affects nearly 6 million people in the U.S. and 700,000 people in Canada. In both countries, Asians are the fastest-growing population but so far they've been vastly underrepresented in Alzheimer's research.
This reality has inspired the launch of the Asian Cohort for Alzheimer's Disease (ACAD), the first Alzheimer's cohort study focused on Asian American and Asian Canadian older adults over time.
SCEI and the University of Southern California have joined forces as one of eight recruiting sites nationwide for ACAD, which seeks to develop more reliable diagnostics and risk predictions, such as biomarkers. The ultimate goal: better treatments and health delivery for Asians in the U.S. and Canada affected by Alzheimer's.
Dr. Rohit Varma, SCEI Founding Director, also serves as an ACAD investigator. He has led research for over three decades aimed at understanding the burden and impact of eye disease on minority groups. His population based research includes The Chinese American Eye Study, the largest such investigation in the world.
To enroll in the ACAD study, visit acadstudy.org.
AI: New Medical Partner in Eye Care
With accelerated development over the past decade, artificial intelligence (AI) is transforming global eye health, says the World Health Organization.
What is AI? Simply put, technology that enables computers/machines to simulate human learning, comprehension, problem solving, even decision making.
What grade does AI get so far?
- AI is gaining credibility in diagnoses. AI algorithms help physicians to predict risk and possible progression of eye conditions and to interpret complex eye scans. So far, AI has performed as well as or better than ophthalmologists in such tasks as detecting diabetic retinopathy and glaucoma.
- AI is becoming a true medical partner. AI can quickly review a patient's medical history and other data to aid physicians in developing personalized treatment plans for conditions like glaucoma, where early intervention matters.
- AI promises to enhance surgical precision. During cataract surgery, AI programs can analyze data to help surgeons plan exact incisions and lens placements.
- AI can help improve access to eye care, particularly in countries with scarce resources. AI-powered telemedicine can link patients to eye care specialists and help screen people at risk for vision loss.
Despite these talents, AI's unlikely to replace eye care doctors. The human touch—including empathy, compassion and complex decision making—is a powerful tool.
At SCEI, we're excited by these developments as we call on technology in ways that benefit our patients most.
Glaucoma Breakthroughs
New research into glaucoma is exploring novel drug delivery systems, game-changing devices and regenerative therapies. The shared goal of these innovations: to lower intraocular pressure (IOP) and prevent damage to the optic nerve.
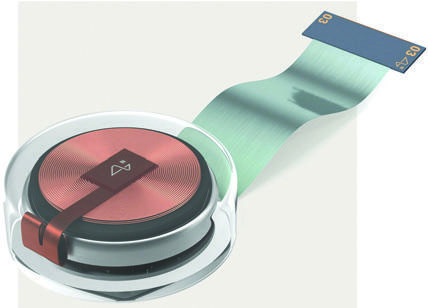
Dr. Rohit Varma, SCEI's Founding Director, recently became the first glaucoma surgeon in the world to implant a next-generation glaucoma drainage device, known as the Calibreye System, into a human patient. The landmark device offers the capability to individually customize glaucoma management unlike anything else until now.
Nearly 66 million people worldwide are affected by glaucoma. More than one-third have moderate to severe glaucoma, putting them at increased risk for blindness.
With the Calibreye System, a glaucoma specialist can manually control the increase and decrease of fluid drained from the eye in glaucoma patients to reduce IOP. High IOP is a leading cause of irreversible vision loss.
«Unlike other drainage devices, the Calibreye System has the potential to achieve personalized, optimal IOP with simple, in-office adjustments,» said Dr. Varma. «I believe this is a transformative advance in the personalized management of our patients with moderate and severe glaucoma.»
Helping blind people see
A device developed by Elon Musk’s brain chip company Neuralink could potentially allow blind people—even those born without the sense of sight— to see. In September 2024, «Blindsight» received «break - through device» designation from the U.S. Food and Drug Administration, which could help speed up development and reviews.
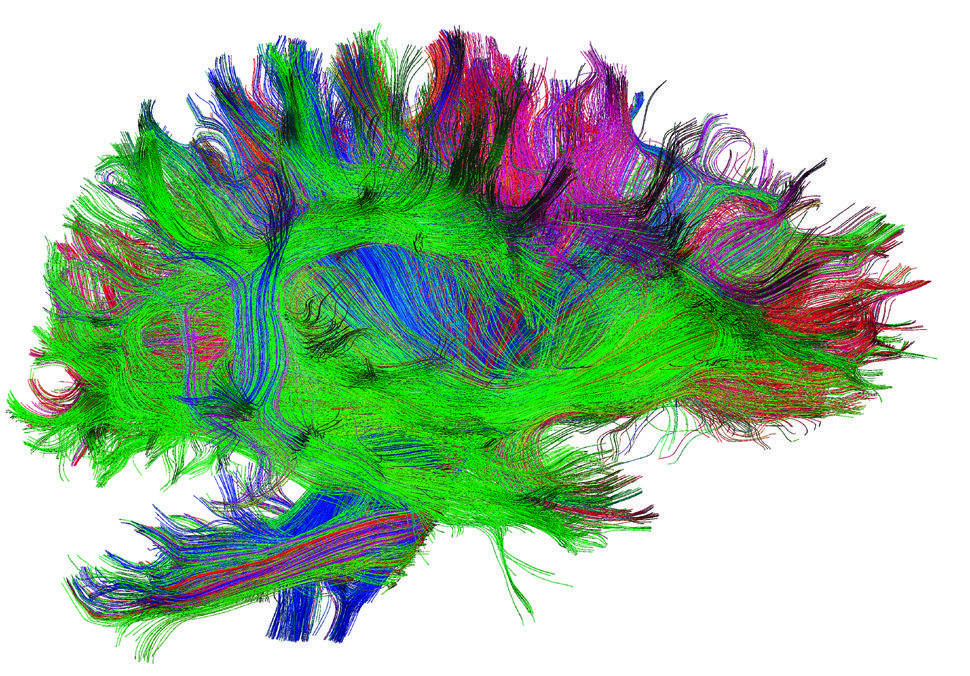
Musk said Blindsight will enable people who have lost both eyes and their optic nerve to see as long as the visual cortex — the part of the brain that receives and processes visual information from the eyes— is intact.
The device uses a chip that processes and communicates neural signals that could be transmitted to devices such as a computer or phone.
Initially, vision will be low resolution, said Musk. But, he added, «eventually it has the potential be better than natural vision.»
Refractive Errors: Identifying Need
A study of visual impairment in African Americans by an SCEI research team has found that about 1 of 7 individuals has an uncorrected refractive error and at least 1 of 20 is not getting their refractive issues addressed.
A refractive error—the most common vision problem worldwide—makes it difficult to see clearly. It happens when the shape of your eye keeps light from focusing accurately on the retina (light-sensitive tissue in the back of the eye).
The most common errors are near-sightedness, far-sightedness, astigmatism (blurred vision), and presbyopia (inability to focus on nearby objects).
The SCEI team, led by first author Nathan Dhablania, MS (and MD/MPH candidate), analyzed findings from 6,337 participants in the African American Eye Disease Study (AFEDS) from 2014-2018. The largest epidemiologic eye study among African Americans to date, AFEDS was led by SCEI Founding Director Rohit Varma, MD, MPH, who is Dr. Dhablania’s mentor.
The study of refractive errors appeared in the April 2024 JAMA Ophthalmology.
«Given the relatively inexpensive and easy intervention of refraction and provision of refractive correction, » the investigators wrote, «it may be possible to reduce this leading cause of visual impairment in this vulnerable segment of the U.S. population.»
Upcoming Events
Community: Access to Eye Care Critical

Approximately 12 million people over 40 in the U.S. have vision impairments, including 4.2 million whose impairment is uncorrectable. This includes 1 million with blindness.
Research has identified four major barriers to eye care among Americans—cost, accessibility, eye health literacy and communication, Healio.com reported.
One solution being looked at to improve vision equity is telehealth. Another is more rural eye clinics. Both can help reach patients, but they can’t handle all eye care needs.
The Southern California Eye Institute (SCEI) is tackling the problem of accessibility on wheels. Our mobile teams go on the road to provide screenings and early detection of eye diseases for people of all ages in underserved areas of Los Angeles.
The SCEI Vision Van’s next stop will be a Community Health Fair on Saturday, Nov. 9, from 9 am – 1 pm at the CHA Hollywood Presbyterian Medical Center (CHA HPMC) at 1300 North Vermont Ave., Los Angeles, in the Visitor Parking Lot.
The Community Health Fair will feature a variety of free community health resources, including vision screening, flu shots and COVID-19 vaccines. The Fair is hosted by CHA HPMC in partnership with Seoul Medical Group and SCEI.
A Better Lens for Cataract Patients
The new OmniVu™ IOL System from Atia Vision—based on a novel modular, shape-changing intraocular lens(IOL)—is filling a need for better solutions for patients with cataracts, which impact nearly 65 million people globally and can lead to blindness.
The clear, permanent artificial lens is implanted during normal cataract surgery. IOLs can improve your vision by correcting such issues as nearsightedness, age-related farsightedness and astigmatism. They also reduce dependence on glasses or contacts.
The OmniVu IOL achieved promising outcomes in its first in-human clinical trials, reported in May 2023, due to its ability to mimic the eye’s natural facility to focus at all ranges—near, intermediate and distant.
A full 100% of trial participants had distance-corrected vision of 20/20 or better six months after surgery and improved vision at intermediate distances (such as using a digital device). Participants also experienced stable vision up to two years and good contrast sensitivity, which means being able to distinguish objects from their backgrounds.
The OmniVu has two basic parts: a shape-changing base lens to provide sharp vision from near to far and a front optic lens that allows the surgeon to customize the lens for each patient’s needs.
Dr. Rohit Varma, SCEI Founding Director, participated in OmniVu’s design and the initial human studies. Atia Vision is moving forward with plans for additional clinical trials

 ENGLISH
ENGLISH  РУССКИЙ
РУССКИЙ 


